Adanna Opara (Lead Writer)
Increasing evidence suggests that quality care prevents a significant number of maternal deaths and disability. High-quality care is also the foundation for improved maternal and neonatal health outcomes. According to the World Health Organisation, despite the fact that more women are giving birth in health facilities than ever before, there has still been no significant increase in maternal and infant the survival rates, which is attributed in part or whole to poor quality care in health facilities.
In Abakpa, Kaduna State, Nigeria, a young mother has just given birth. She described the care she received throughout her labour and delivery at a hospital in Giwa. “Immediately I came to the hospital, I was taken to the labour ward, given a bed, and my BP and everything was checked… My contraction wasn’t much, so I was placed on drip and some treatment. Within a moment, I gave birth. Immediately I gave birth; the baby was placed on my chest for me to start breastfeeding after some minutes…I like the way they attended to me,” she shared.
According to the Lancet Commission on High-Quality Health Systems (2018), a strengthened health system that provides high-quality maternity care might prevent half of all maternal and 1 million newborn deaths each year. For this young mother, her childbirth experience was safe, as a result of the quality of care she received.
The SafeCare Methodology of Quality Improvement
Emphasising that quality care is the key to reducing maternal mortality in Nigeria, Pathfinder Nigeria and PharmAccess Foundation collaborated with the Kaduna State Ministry of Health to improve the quality of maternal health care in twenty-five (25) private health facilities through the Saving Mothers, Giving Life (SMGL 2.0) project.
The SMGL 2.0 project, implemented in Kaduna State between 2020 and 2023, sought to improve access to and quality of maternal and newborn health services and strengthen collaboration and partnership between the Kaduna State Ministry of Health and the private health sector. The project also worked with traditional birth attendants to improve women’s health-seeking behaviours, referrals and health insurance enrolment. To strengthen accountability for maternal deaths, strategies utilised included the establishment of the Maternal and Perinatal Death Surveillance and Response and the deployment of an interactive digital health chat solution on WhatsApp (AskNivi) in partnership with Nivi to provide relevant maternal and newborn health information to pregnant women.
In improving quality care in the facilities, the project utilised the SafeCare methodology to strengthen the facility’s capacity to provide Emergency Obstetric and Newborn Care (EmONC) and family planning services.
SafeCare is an internationally accredited methodology based on the WHO quality of care framework developed to improve the quality of care in health care settings, (especially in low- and middle-income countries (LMIC)), by implementing a set of standards. These standards are broken down into achievable and measurable steps to facilitate incremental quality improvement.
The SafeCare standards cover both medical and non-medical aspects of care and are structured around four (4) broad service elements: management, clinical, clinical support and ancillary. These four service elements are further divided into 13 categories. A health facility’s performance is measured against the SafeCare standards, and it is awarded a certificate of improvement based on its performance. There are five (5) levels of quality certifications that a health facility can attain under the SafeCare programme, ranging from level 1 (very modest quality) to level 5 (high quality).
In the project’s first year, facilities were assessed using SafeCare digital tools to obtain a baseline of the quality of care delivered in each facility. Based on the assessment, 17 of the 25 health facilities fell under level one while the remaining eight were placed on level two. Automated assessment reports, and quality improvement plans (QIP) were then generated and shared with all 25 facilities.

Following the assessment, selected staff of each of the 25 health facilities were appointed as Quality Improvement (QI) teams. The QI teams received training on the interactive Quality Improvement Platform for Providers (QIPP) and were responsible for guiding the facilities on downloading the quality-of-care standard operating procedures (SOPs) from the QIPP, customising the SOPs for specific facility use, implementing priority activities reflected in the QIPP, and reporting on all QI activities implemented, including picture evidence, into the SafeCare platform.
The SMGL 2.0 team provided quarterly on-site supervision and virtual mentoring to the 25 facilities, and feedback was used to further improve the quality of care provided by each facility. During the quarterly supportive supervision visits, the SMGL team addressed challenges faced by the QI teams or facility staff in implementing the SafeCare model. Recommendations were made, and the implementation was tracked during subsequent visits.
In the project’s second year, a second assessment was conducted. Results from the assessment showed that 12 facilities moved up to a higher quality level (e.g., from level 1 to level 2 or from level 2 to level 3), seven (7) facilities moved up two levels, i.e., from level 1 to level 3, while five (5) remained on the same level. It appears that the act of baselining and measuring quality of care is a motivator to improve.
SafeCare for maternal health
The SafeCare methodology also equipped health care providers in supported facilities with skills, tools and resources to provide quality care to pregnant mothers.
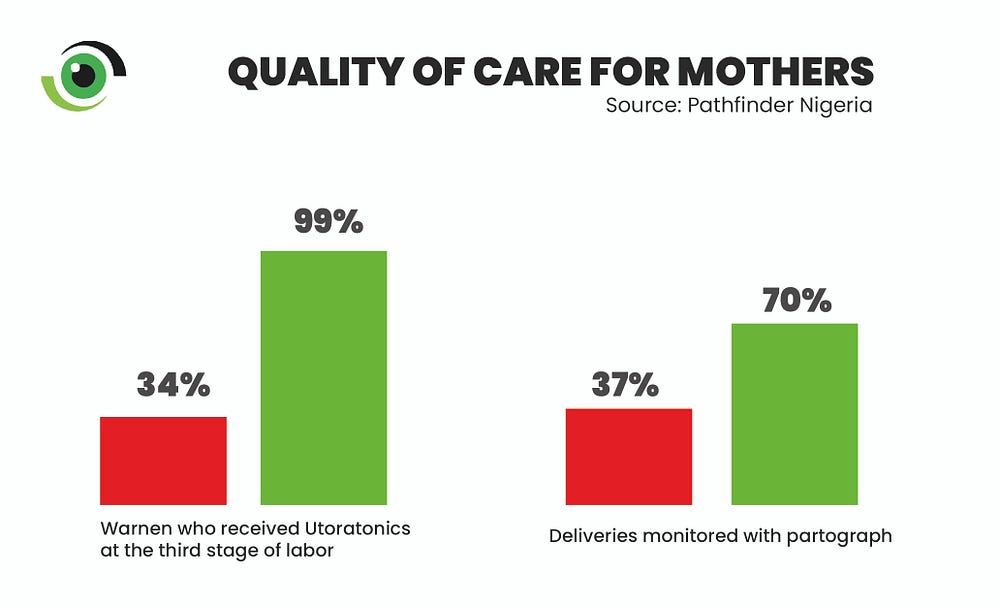
A health care worker at a hospital in Giwa, Kaduna shared how the training she received built her capacity to provide quality maternal health services to pregnant women. “We had the knowledge of all these things, but you know, after the exposure we had at the training, it was as if we never knew anything. We now have more effective solutions to better manage excessive postpartum bleeding through the active management of the third stage of labour…through the training, we have been equipped to promptly detect complications in labour and depict it in a partograph,” she said.

The health worker passed her learnings from the training on to other facility staff and noted that everyone is working as a team to ensure positive maternal outcomes “ all of us are able to detect or identify when we see the partograph is not in order, …and we always act faster now with the use of partograph,” she added.
Results from the end-of-project assessment attest to the quality improvement efforts, showing that maternal and perinatal deaths in all 25 private health facilities decreased by 60% and 16%, respectively, while the percentage of newborns with birth asphyxia that were successfully resuscitated increased by 36%.
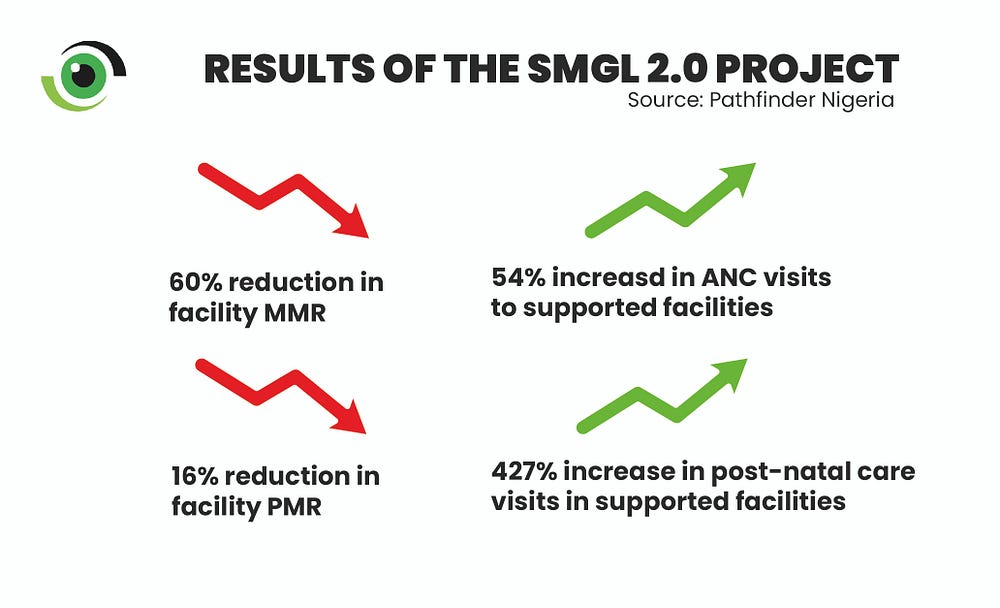
Partograph-monitored deliveries increased by 33% and births in supported facilities increased by 17%. There was a 52% reduction in stock-outs of essential medicines while there was a 65% increase in women who received active management of the third stage of labour.
Not without a few hitches
One key programmatic challenge was the high attrition rate of health care providers in the private facilities. Out of the 438 health care providers who were trained, 93 (21%) resigned their services to take up new opportunities. To mitigate this, the project ensured that key staff, such as the hospital’s owners and managers, were trained, and the training was stepped down to other staff within the facilities.
Additionally, building collaboration and partnership between the facilities and the Kaduna state government initially came with some level of suspicion from the private sector. This was addressed by engaging in continuous advocacy between the government and the private health sector. According to Paulina Akanet, State Program Manager, SMGL 2.0 project, Pathfinder Nigeria, the project involved private sector associations including the Association of Nigerian Private Medicare Practitioners (ANPMP) and Association of General & Private Medical Practitioners (AGPNP), in technical working group meetings within the state to ensure inclusivity and informed discussions.
Why focus on quality care
Quality care is critical to improved outcomes for maternal and newborn health. The adoption of a quality framework such as the SafeCare methodology under the SMGL 2.0 project in Kaduna state provides clear evidence that quality of care and maternal health outcomes can be improved if the capacity of private health facilities is strengthened using a quality improvement model.
Scale-up and replication of this model to more private and public health facilities in more states across Nigeria would bring us closer to attaining the SDG 3.1 global target of having less than 70 maternal deaths per 100,000 live births.
This program is supported by funding from MSD, through MSD for Mothers, the company’s global initiative to help create a world where no woman has to die while giving life. MSD for Mothers is an initiative of Merck & Co., Inc., Rahway, NJ, U.S.A
K Fosu The Informant is a lifestyle blogger with 6 years' experience in content and web development. He is a Google keyword planner, SEO analyst, an influencer and entrepreneur who holds BA Degree from Ghana's Premier University.



